Lighting a Path for Improved Cancer Treatment
Sometimes researchers quickly connect the dots that help advance medicine. That seems to be the story of Cornell dots — or C-dots — the silica nanoparticles that are lighting a path toward improved cancer imaging and drug delivery. Where other methods have failed, these fluorescent C-dots (see box) have been shown in animals to safely light up cancer cells, track their movement and then quickly exit the body. Michelle Bradbury, M.D., Ph.D., a clinician-scientist at Memorial Sloan-Kettering Cancer Center (MSKCC) in New York City, will test multimodal C-dots in humans for the first time. She believes that imaging metastatic tumors with these tiny particles could one day help surgeons better define tumor borders, find diseased lymph nodes, and see where cancer has spread in patients' bodies for targeted tumor therapy — all in one platform and without negative side effects.
Bradbury credits innovative funding and a diverse team of experts at both MSKCC and Cornell University with facilitating her research and expediting a usually lengthy research process. By joining forces with C-dot creator and Cornell materials science engineer Ulrich Wiesner, Ph.D., she tapped into nearly a decade of C-dot research and nanoparticle expertise.
Touched personally by cancer, Wiesner was surprised by the few methods doctors had to visualize the full extent of cancer cell invasion into the body's tissues. Inspired by millions-of-years-old microscopic ocean life whose leftover silica exoskeletons cover the planet, Wiesner believed silica to be biologically safe or evolution would have discarded it long ago. He thought this inert material could be engineered in a way to look at cancer.
An Unlikely Collaboration Bears Fruit
Bradbury wanted to target tumors and selectively treat them with a variety of new drugs. When she contacted Wiesner in 2006, he and his colleagues already had synthesized small particles that could clear through the kidneys. However, they lacked specific evaluation data required by the U.S. Food and Drug Administration (FDA) for clinical use. Moreover, Bradbury wanted to develop a tumor-selective particle, so they obtained a pilot grant from the Weill Cornell Medical College Clinical and Translational Science Center (CTSC), which is supported by NIH's Clinical and Translational Science Awards (CTSA) program. CTSA institutions, like Weill Cornell, encourage collaborative teams of diverse investigators to tackle complex health issues and then translate their discoveries into practical solutions for patients.
As Julianne Imperato-McGinley, M.D., principal investigator of the CTSC, explained, "This was a novel idea with tremendous potential." To fund a pilot research project, the CTSC requires collaboration among different disciplines and consortium institutions. "These investigators met and wanted a way to collaborate, fitting our requirements perfectly."
"This was a seed grant," Wiesner said. "You hope that any seed you plant will grow, and that is precisely what happened here. We might never have talked otherwise."
The best way for the body to eliminate particles efficiently is through the kidneys, and that means the particles must be very small. The investigators tested two sizes, 3.3 nm and 6 nm. (A nanometer [nm] is one-billionth of a meter. If the particles had a diameter of 10 nm and were lined up single file, it would take more than 2.5 million to make a line one inch long.)
To be useful, the particles also needed to make whatever they cling to visible. The investigators put a tiny amount of a near-infrared fluorescent dye within the C-dot. This makes the dots light the way as they pass through the body. Silica is a very rigid material, so it squeezes the dye in the dots, making it shine much more brightly than if it were free.
The first test in mice proved successful. When excited by the right light, the dots shone brightly. This made it possible to see them in the bladder to verify that the rodents excreted nearly all of them within 48 hours with no toxicity or ill effects.
In successive experiments, Bradbury's colleague Oula Penate-Medina, an MSKCC nano- and radiochemist, attached radioactive iodine to the particles to make them detectable by positron emission tomography (PET) imaging. Hybrid Silica Technologies, Inc., the supplier of the particle, attached a short sequence of amino acids (the building blocks of proteins) called a cyclic RGD peptide, which binds to cancer cell surface receptors, and found that the C-dots attached to melanoma cells very effectively.
"This seed grant came along at the perfect time to help us get the data we needed," Bradbury said. "It funded the studies that ultimately gave us a jump-start toward the clinic." The next step was to submit an Investigational New Drug (IND) application to the FDA.
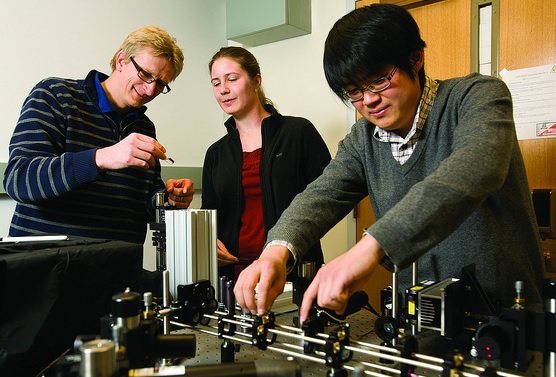
Cornell University materials science engineer Ulrich Wiesner (left) and graduate students Jennifer Drewes and Kai Ma characterize the size and brightness of Cornell dots (C-dots) in research to improve cancer diagnosis and treatment. (Cornell University Photo)
The Jump to the Clinic
In a textbook case of translational research, this unlikely collaboration across institutions — bridging the gulf between materials science and biomedical research — has taken multimodal C-dots through regulatory hurdles and into their first-ever clinical study with patients.
With permission from the MSKCC Institutional Review Board, Bradbury is now recruiting five melanoma patients who will each receive an injection of C-dots. "We plan to take serial PET scans over a couple of days, sample blood and urine, and determine where the particles are going," explained Bradbury.
Another purpose of the trial is to test the safety of C-dots and to ensure that they leave the body efficiently through the kidneys. "Once the study has been completed in these patients, we can spring forward to perform tumor-targeting," said Bradbury. "And, in future therapeutic studies, we will attach drugs or immune components to the particle."
If all goes according to plan, the researchers will evaluate the use of this tumor-selective multimodal particle for clinical "sentinel node mapping," determining which lymph node is the first to receive cancer cells if a tumor already is spreading. This is a crucial first step in determining which, if any, lymph nodes must be removed. Not getting rid of enough lymph nodes can mean a patient's death due to metastatic disease. Taking too many may cause unwanted fluid accumulation, affecting a cancer survivor's quality of life.
"Using both optical and PET imaging, we can sensitively track the C-dots in real-time as they rapidly go to the nodes," said Bradbury. Using a hand-held fluorescent camera system, surgeons can trace the fluorescence signal from lymph nodes that contain the metastatic disease. With another device that detects radioactivity counts, they can confirm the results. Armed with this data, physicians then select treatment options. "One very attractive feature is being able to control a drug's distribution by binding it to the particles," Bradbury added. "What is not taken directly to the cancer cells will be passed out through the kidneys." This could reduce toxicity to vulnerable organs and combat cancer's notorious ability to become resistant to drugs.
A Vision for the Future
Wiesner is emphatic: "I want to reiterate the idea that once we know the particle is safe and working, we can move toward personalized medicine."
"In the future, instead of treating patients with drugs based on their body weight," Bradbury added, "we can optimize treatment by controlling drug dosing to target the cancer. This is the essence of individualized care."
Multimodal C-dots could offer this promise. Using PET to track radiolabeled drugs bound to the particle, doctors could see how much of the drug is taken up by a patient's tumor. Coupled with other key tumor characteristics, physicians could select dosing regimens designed for treating individual tumors. In addition, surgeons could use the technology to see where metastatic disease has spread and target therapies based on the cancer's stage.
"There is a lot of enthusiasm among clinicians for using such multimodal platforms," said Bradbury. "This particle will make it possible to improve both diagnostics and treatment."
Bradbury believes CTSC pilot funding was essential, explaining that even the best idea will not be funded without some pilot data to back it up. "It is not typical for something like this to go into the clinic," she said. "The CTSC award allowed us to fund our approach and complete the essential studies needed for the IND proposal within a two-year period." She plans to use the CTSC to help her coordinate multicenter patient studies as her research progresses.
"This is a beautiful example of what the CTSC exists to do," Imperato-McGinley added. "We try to encourage collaborative, multidisciplinary research because the fruitful mixture of ideas and approaches from different disciplines works. For the two of them to get this far in such a short time is amazing."
Posted March 2012